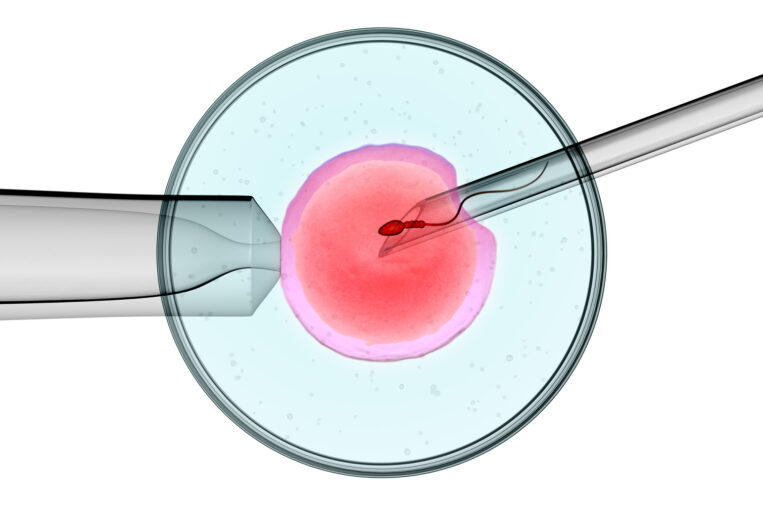
A study suggests that the common worry that Intracytoplasmic Sperm Injection (ICSI) increases genetic defects isn’t the case and that poor sperm quality is the primary culprit.
Patients are often worried about whether the use of intracytoplasmic sperm injection (ICSI) performed with in vitro fertilization (IVF) cycles increases the risk of genetic abnormalities. A study reported in the journal Fertility and Sterility (Coates et al) is perhaps the most reassuring to date that the process of ICSI itself does not increase the risk of genetic abnormalities.
The study involved genetic analysis of 3,835 embryos from six groups of patients undergoing IVF, three groups of patients using their own eggs (average female age was 35), and three groups of patients using donor eggs (average age of egg donor was 25). Both groups, own eggs and donor eggs, were further divided into three additional groups of patients: those doing conventional IVF insemination of eggs, those doing ICSI where the male partner had a very low sperm count (< 5 million per ml), and those doing ICSI with sperm of normal count.
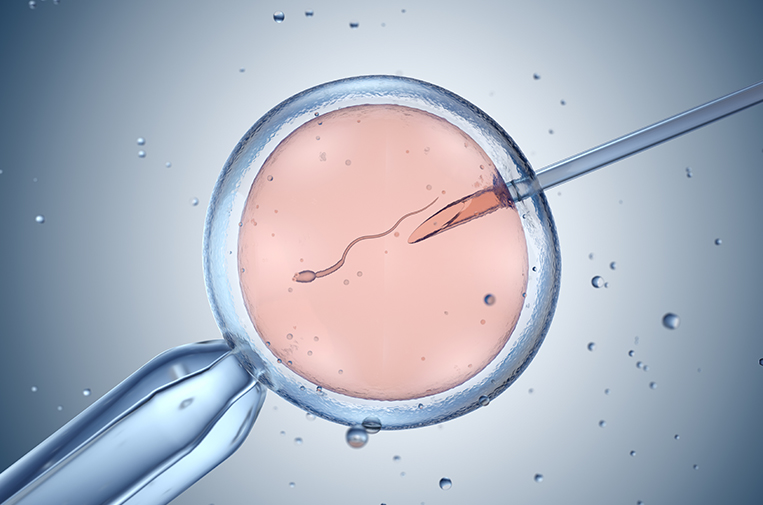
Problems from poor sperm quality, not ICSI
Finding: The study found that in both egg donor and own egg groups, with sperm from males with very low sperm count that used ICSI, the percentage of genetic abnormalities in the embryo’s sex chromosomes (X and Y) was 3 times higher than the groups with normal sperm count that used both conventional insemination and ICSI. There was an average of 2 percent abnormal embryos in the group with normal sperm count and 6 percent abnormal embryos in the low sperm count group.
What does this mean? This strongly suggests that it is not the ICSI procedure itself but rather the suboptimal genetic quality of sperm that increases genetic abnormalities. Most genetic abnormalities found in the sex chromosomes are derived from the sperm, not the egg. Men with very low sperm counts (< 5 million) are known to have a higher percentage of genetically abnormal sperm.
Finding: Genetic abnormalities in the 22 non-sex chromosomes are more often derived from the egg. In this study, there were no significant differences in genetic abnormalities in non-sex chromosomes in the groups with conventional insemination, ICSI, or ICSI with very low sperm count. However, when you compare the percentage of embryos with genetic abnormalities in non-sex chromosomes, there were twice as many abnormalities in the group using their own eggs (average female age 35) as there were in the group using donor eggs (average donor age 25).
What does this mean? We know that it is the age of the egg provider that predicts the non-sex chromosome genetic abnormality rate in the embryos.
In conclusion, this study is very reassuring that the ICSI procedure itself not increasing risks of genetic abnormalities unless the sperm count in the male partner is very low. When the sperm count is extremely low (< 5 million), patients may want to consider pre-implantation genetic screening (PGS) of embryos to reduce the risk of transferring a genetically abnormal embryo.