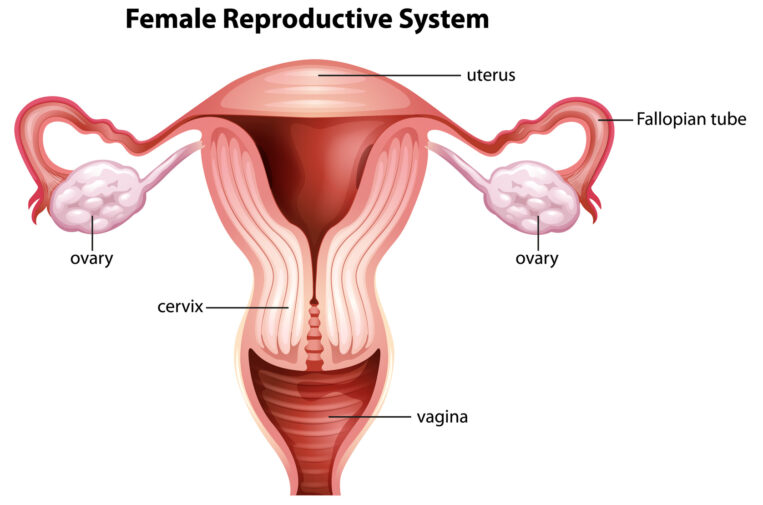
Ectopic pregnancy (a pregnancy outside the womb and in the wrong place, such as the fallopian tube or ovary) is still a life-threatening complication. While in vitro fertilization (IVF) is recommended for women at risk of an ectopic pregnancy, especially if they’ve already had more than one ectopic pregnancy, it is not a 100 percent guarantee that a woman will not have an ectopic pregnancy.
Why? As many of my patients ask.
Although in IVF the embryo is placed in the uterus, generally 1.8 cm from the top, the waves of uterine contractions can propel the embryo backward through the fallopian tubes before it actually implants. This means there are still approximately 12-24 hours in which the embryo can move before implantation begins. It has also been surmised that damaged tubes can suck the embryos back into them due to pressure differentials between the uterus and the tube.
So you will find it reassuring to note that recent statistics on ectopic pregnancies (also called tubal pregnancies) after embryo transfer are on the decrease. It declined from 20 to 12 per 1,000 assisted reproductive cases over the last 12 years in the United Kingdom. It now occurs in less than 2 percent of natural (spontaneous) pregnancies and 1.4 percent of IVF and IUI pregnancies.
But this risk can be subdivided even more, providing reassurance for those without tubal disease. There is now known to be a 3 percent risk if a patient has tubal infertility and more than one embryo is transferred, but only 0.8 percent if the patient has male factor infertility and only one embryo is transferred. The statistics are similar in the U.S. showing a decline in ectopic pregnancies with IVF from 2 to 1.6 percent and a reduction in risk from 2.5 percent, if four embryos were transferred, down to 1.6 percent if only one embryo was transferred, regardless of the embryo stage.
The most common causes of tubal factor infertility include sexually transmitted infections with chlamydia, abdominal surgery, endometriosis, and smoking.
Lowering the total number of embryos transferred and transferring at the blastocyst stage (day 5) are thought to be the reasons for the decrease. Reproductive Science Center has long been a strong advocate of elective single embryo transfer (eSET) and leads the network in helping patients achieve high success rates while transferring fewer embryos. RSC has also been performing blastocyst transfers for the majority of our patients for over 10 years, giving us very low ectopic pregnancy rates.
Early detection of an ectopic pregnancy is critical. So, serial monitoring of human chorionic gonadotropin (hCG) levels and early ultrasounds at six weeks estimated gestational age (two weeks after finding out you are pregnant) can help to manage ectopic pregnancies safely 95-98 percent of the time, avoiding the need for surgery.